As part of our ongoing commitment to expanding convenient care, we’re excited to announce the launch of Solv Revenue Maximizer, a new patient experience enhancement that reduces claim denials, speeds up patient payment, and decreases bad debt.
Up to 22% of claim denials are caused by errors in registration and verification. Revenue Maximizer automatically corrects and verifies 96% of addresses, improving EHR data and saving your team manual error corrections. It automatically reads insurance card text, prevents EHR duplicates, and prompts patients to pay by text—so you get paid faster.
Prevalence of claim denials and bad debt
Most of the work in healthcare to bill and collect revenue is done after the patient has left the building. Unfortunately, billing and collection problems are all too common due to inaccurate patient data and errors that begin during registration at the time of visit.
In fact, according to NCG medical, most medical practices have a 75%-85% first pass clean claim rate, meaning that at least 15-25% of claims require more time to rework the claim from staff. Many of these errors are caused by small mistakes in registration or verification, with Change Healthcare estimating 22% of denials are caused by errors in registration and verification, and another 12% of denials caused by missing or invalid claim data.
Given all these issues, providers rely on their billing teams and revenue cycle management companies to help with back-end billing and bad debt collections. However, they don’t have the capability to increase revenue efficiency on the front end, where many of the errors begin.
Introducing Solv Revenue Maximizer
At Solv, we believe that the best way to improve revenue and minimize write-offs and denials from the time of booking is by getting data right the first time – straight from the patient and their digital insurance card.
By improving data accuracy throughout the RCM front-end workflow, Solv Revenue Maximizer aims to free up staff time and reduce claim denials and bad debt during the billing process.
How It Works:
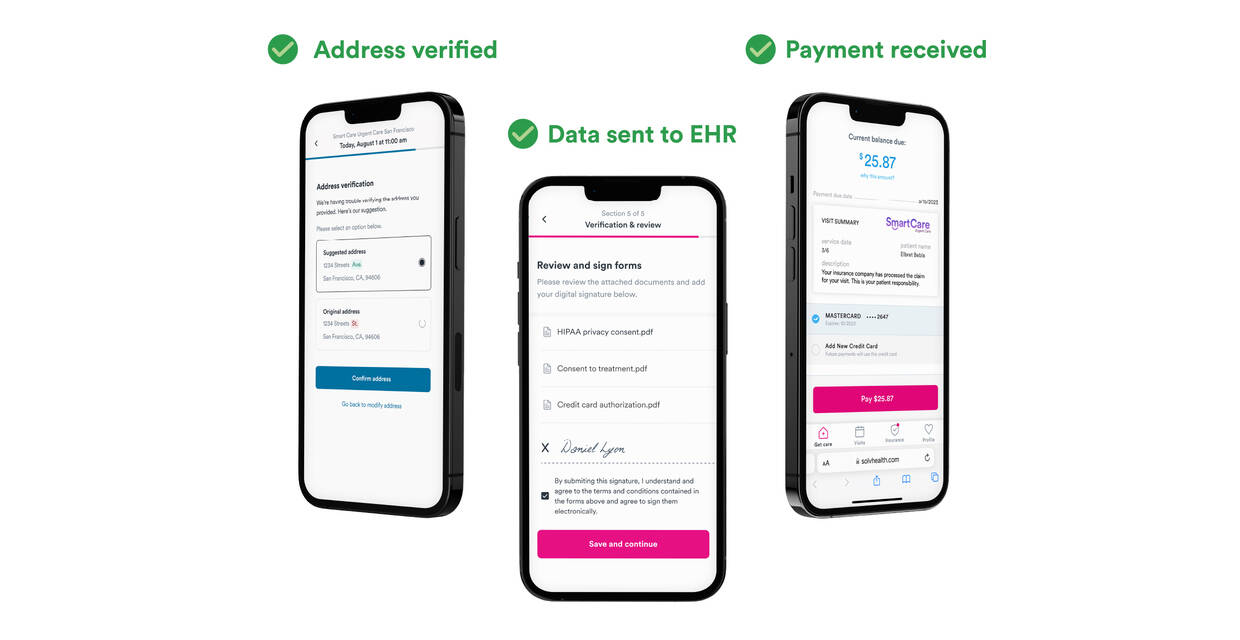
Automatic data correction reduces claim denials.
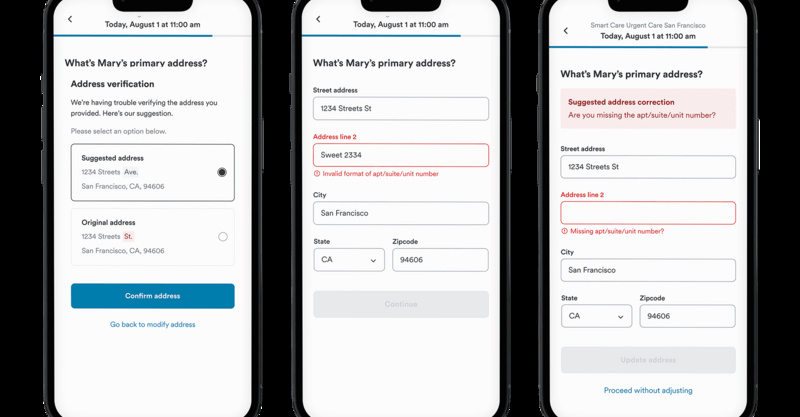
Registration validation
Automatic address correction and real-time insurance verification improve patient data and reduce claim denials.
- Address validation: automatically catches address errors, or missing information like apartment numbers.
- Insurance OCR: OCR technology converts insurance card photos into text instantly, reducing manual entry error.

Duplicate prevention
EHR transfer check reduces duplicate records and saves tedious correction work for you for your billing team.
- Data autofill: patient details are saved and auto-filled in the future
- EHR transfer check: when a patient isn’t matched, they are automatically flagged for the front desk to validate

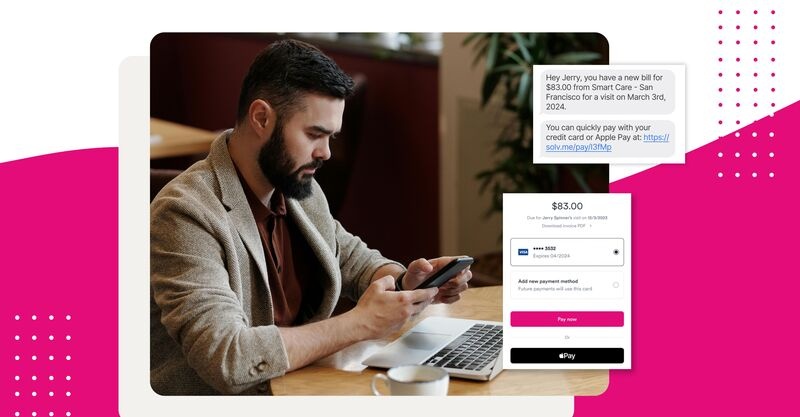
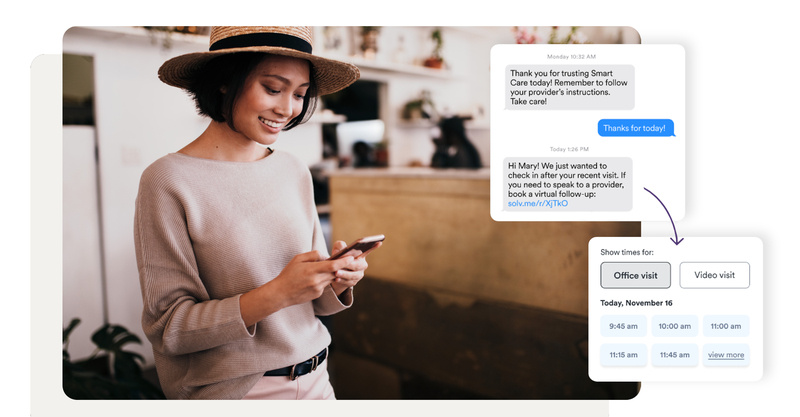
Mobile technology speeds up patient payment and reduces bad debt.
Text-to-pay
Text messages and mobile friendly payment options allow you to get paid faster and reduce bad debt while providing an easy-to-use payment experience for your patients.
- SMS bills: sends a bill via text instead of relying on mail, also saves on postage and handling fees
- Mobile checkout: patients pay quickly on their phone, and pay with a saved credit card

Solv Revenue Maximizer improves data in your EHR through integrations with top EHRs including Athena, eClinicalWorks, AllScripts, Nexgen, Cerner, and Epic as well as automatic and seamless data transfer into Experity.
Ready to improve your revenue cycle management? Check out Solv.